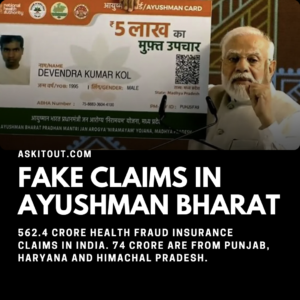
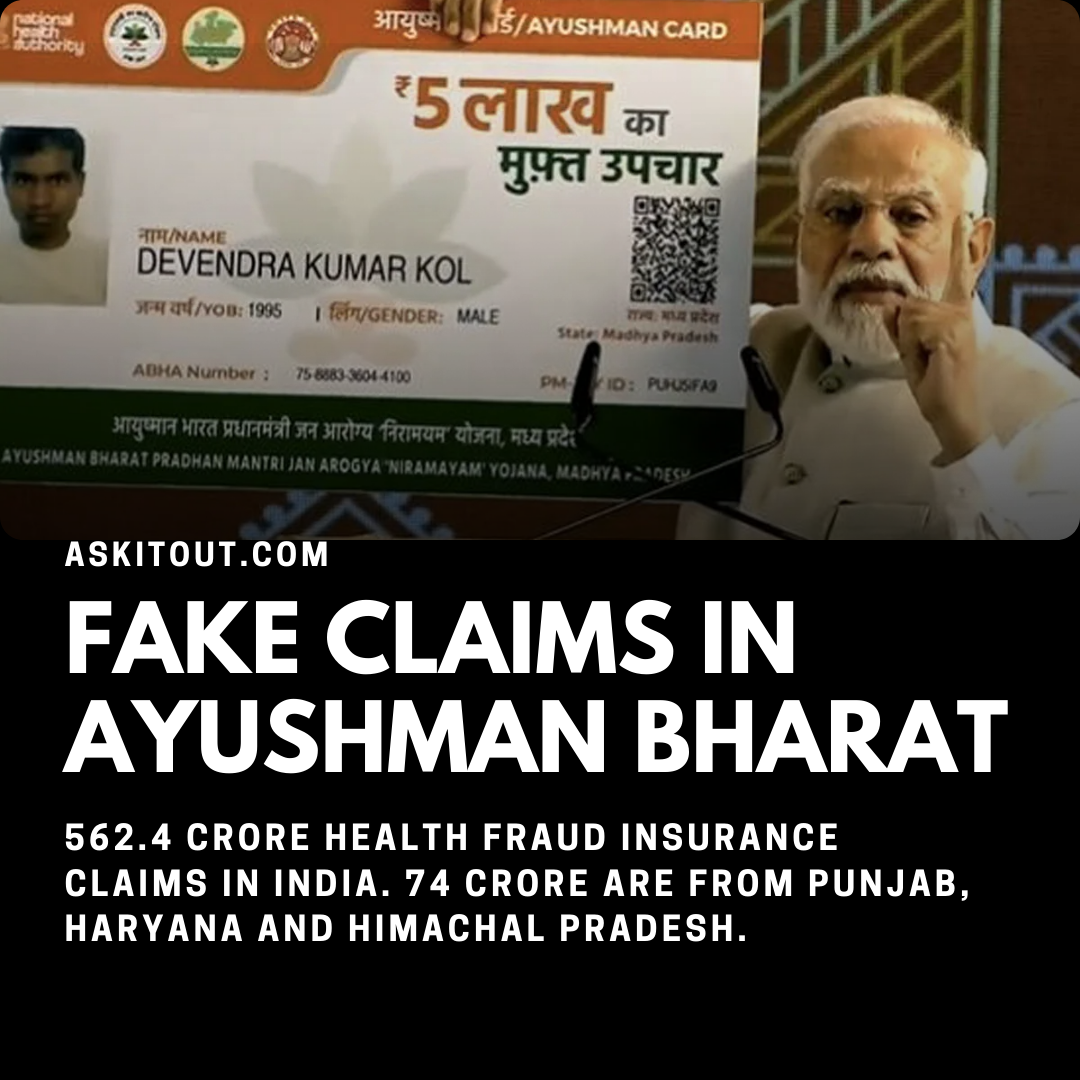
A large-scale fraud has been uncovered in the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), with private hospitals inflating insurance claims and misusing the scheme. The states of Punjab, Haryana, and Himachal Pradesh alone account for ₹74.5 crore of the fraudulent claims, making up 13% of the total fake claims detected nationwide.
Key Findings of the Fraud Investigation
- Total Fake Claims Detected: ₹562.4 crore across India
- Punjab, Haryana, Himachal Pradesh: ₹74.5 crore in fraudulent claims
- Breakdown by State:
- Haryana: ₹45.03 crore
- Punjab: ₹28.7 crore
- Himachal Pradesh: ₹75.65 lakh
Additionally, thousands of beneficiaries were found registered under a single mobile number, raising concerns over identity fraud:
- Punjab: 30,001 cases
- Haryana: 13,555 cases
- Himachal Pradesh: 2,892 cases
Government Action Against Fraud
The Union Health Ministry has emphasized a zero-tolerance policy towards fraud and misuse under Ayushman Bharat. Steps taken include:
✔ Blacklisting or suspending hospitals found guilty of malpractice
✔ Rejecting fraudulent claims and imposing penalties
✔ Random audits and surprise inspections to verify hospital claims
✔ AI-based fraud detection systems for real-time monitoring
So far, 1,114 hospitals have been de-empanelled, and 549 suspended for their involvement in fraudulent activities. Advanced technologies like machine learning, image classification, and database monitoring are being used to strengthen fraud detection efforts.
What is Ayushman Bharat?
Ayushman Bharat provides ₹5 lakh per family per year for hospital treatments, covering secondary and tertiary healthcare. Recently, the scheme was expanded to include senior citizens aged 70 and above, regardless of their financial status, under the Vay Vandana Card initiative.
This large-scale fraud highlights the need for stricter monitoring and enforcement to ensure that the scheme benefits the right people while preventing misuse by hospitals and individuals.
References and Information Sources:
- Ayushman Bharat Fake Claims: Rs 562.4 crore fraud health insurance claims in India, 74 crore of them from Punjab, Haryana, Himachal Pradesh | Chandigarh News – The Times of India
- Centre detects fake AB-PMJAY claims worth Rs 562.4 crore – Medical Buyer
1 thought on “Ayushman Bharat Fraud: ₹562.4 Crore in Fake Claims Uncovered”